As podiatrists we see a lot of patients experiencing unsightly discoloured nails. Nail fungus is an extremely common problem which can affect anyone. Luckily, nail fungus can be successfully treated by our Brisbane podiatrists! In this blog we will learn about the common reasons for nail fungus to occur as well as the best treatment for nail fungus.
What is nail fungus?
The medical term for nails affected by fungus is ‘Onychomycosis’ (Onycho: “of the nails”, mycosis: fungal infection). Fungal nails are a type of infection involving the nail bed and plate. This fungus is most commonly a dermatophyte (commonly ‘tricophotin rubin’). It can also involve yeasts like candida albicans.
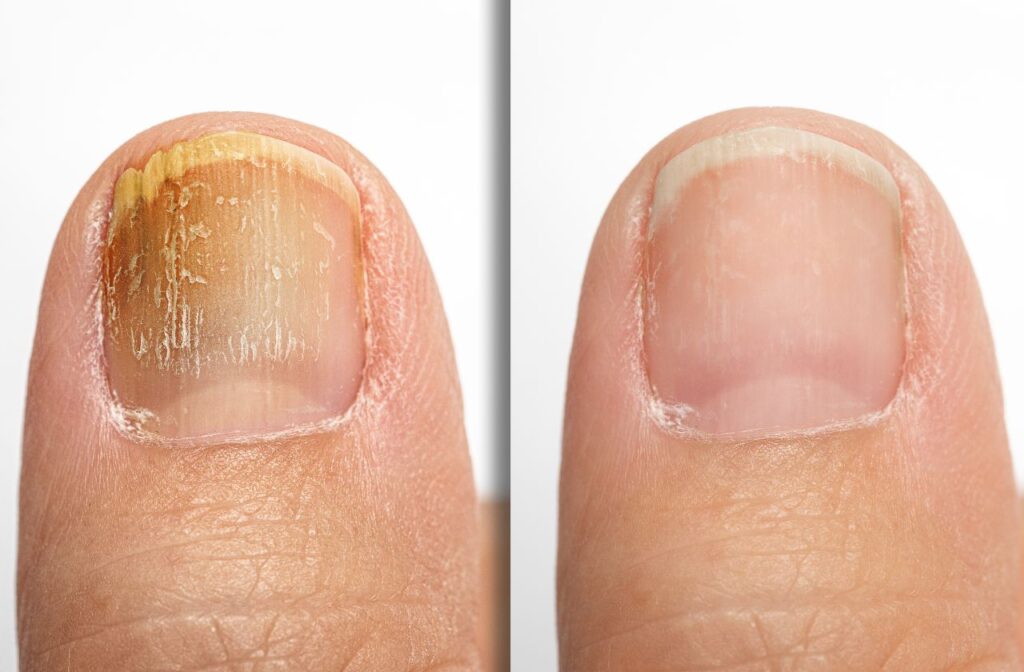
These fungi are extremely opportunistic and find their way onto the skin and nails from the environment. The fungi have a food source from the keratin found in the nail and surrounding skin. This is the cause of the common discoloration, smell and texture changes to the nail. They will often become thickened and crumbly as the fungus eats away at the nail. You will also usually see debris under the nail or the nail may seem to lift up from the nail bed.

What are the different types of nail fungus?
- Superficial White – This type of presentation will typically look like a white powder on top of your nails; pitting will start to occur in these areas.
- Distal-lateral Subungual Onychomycosis (DLSO) – This can present as a white/yellow/brownish discoloration with plaque debris underneath the corner of your nails.
- Distal Onychomycosis – Presents similarly however has some separation and debris under the centre at the tip of the nail.
- Proximal Subungual Onychomycosis (PSO) – Presents at the base of the nail near the cuticle and is often due to people pushing back their cuticles. It will be a yellow/white discolouration with destruction of the nail plate present.
- Total Dystrophic/Candidal Onychomycosis – Often the final stages of a fungal infection. The entire nail has become thickened, crumbly, discoloured and often separated from the nail bed.
What causes a fungal nail infection to happen?
Age
Fungal nail infections are quite common and occur in people of all ages, but most at risk are older adults. This is because as we age, our nails become more brittle and dry. As a result, cracks form in the nails allowing fungi such as dermatophytes, candida or moulds to enter. A weakened immune system and poor circulation also play a role in the likelihood of getting an infection.
Health Status
If you are immunocompromised you are at increased risk of developing a fungal nail infection. Typical health conditions that could increase your risk of a fungal infection are:
- Diabetes Mellitus
- Cancer treatments such as chemotherapy
- Rheumatoid Arthritis
- Skin conditions such as psoriasis, eczema and hyperhidrosis
- Peripheral Vascular Disease
- Trauma to the nail

Environmental factors
Living in an area with a warmer climate and humidity (sorry, Brisbane!) can lead to sweaty feet, which creates a perfect environment for fungus. Combined with this, walking barefoot increases the likelihood of coming in contact with various fungi. The likelihood is increased again when going to more public places, particularly where moist environments can harbor the fungal growth such as: public showers, pools and gyms.

Tinea Pedis (Athlete’s foot)
Fungal nail infections can often develop from untreated tinea, commonly known as Athlete’s foot. While this is a skin infection, it involves the same organisms which can infect the nail. Therefore it is very likely that the fungus from the skin around the nail can enter the nail. This is why it is so important to treat the skin of your feet while you address your fungal nails.
Excess Sweating
Fungi like dark, moist environments. Having sweaty feet can provide the ideal environment for fungus to enter and multiply on the skin or nails. Excessively sweaty feet (hyperhidrosis) can be due to various medical conditions such as hyperthyroidism or anxiety. They can also be due to simple physical causes such as thick socks and non-breathable footwear (particularly footwear with waterproofing).
Best Treatment for Nail Fungus
Although fungal nails can be unsightly cosmetically, they don’t often cause medical problems. However, in some cases the nails can break off and become ingrown toenails, which are at risk of infections such as cellulitis. Some people are at a higher risk of complications from fungal nails too.

Fungal Nail Laser (Lunula)
One of the most innovative fungal nail lasers on the market for treatment of fungal nails is the cold laser known as the Lunula. The Lunula Low-Level Cold Laser uses two specific low-powered laser beams at different ends of the light spectrum simultaneously to destroy the fungus infecting your toenails, in the nail bed and the surrounding skin. It’s painless, safe and effective.
Medical studies have shown that the Lunula cold laser has been able to resolve fungal nails in 96% of cases across 36 weeks.
Blue (405nm) Cold Laser
The first laser is the Blue (405nm) laser. This laser acts specifically and directly upon the fungal cells. It causes changes directly to the outer wall of the fungal cells, weakening it significantly. As the outer wall is what is protecting the fungal cell from the body’s immune system. Damaging and weakening it allows the body’s immune system to attack and destroy the fungal cell for good.
Red (635nm) Cold Laser
The nail is also hit simultaneously with a Red (635nm) laser. This laser acts on the body’s natural immune cells – strengthening them, making them more active and able to kill the weakened fungus. In addition, the red light improves blood flow, bringing nutrients and additional immune cells to the affected area which speeds up the treatment process.
Other treatments
Lacquers and Tinctures
There are various fungal lacquers and tinctures on the market to help in the treatment of fungal nails. Discuss the options with your podiatrist. They can help you choose the best one for your treatment as they all have different cost and effectiveness depending on the severity of the infection.
Additionally, sometimes you may also need a cream for the surrounding skin if it also has a fungal infection.

Oral Antifungal Medication
Available from your General Practitioner with a prescription there are a few different forms of antifungal medications (e.g. Terbinafine tablets). These medications are usually reserved for the most severe and stubborn of nail fungus. Whilst effective, oral medications involve a risk of side effects which must be discussed with your doctor. They are not suitable or tolerated by a percentage of patients. This is one of the reasons many patients of ours chose the Lunula laser as their best treatment options for nail fungus.

Will nail fungus come back?
Nails or feet that are exposed to fungi can be infected again. This is much like how you can sprain your ankle multiple times through trauma. This is why we always focus on education and the after-care of our patients.
Reinfection can occur if fungal spores are still in the socks or shoes you are using. Also if you continue exposing the nail to the fungus that infected it in the first place. That is why when having a Lunula laser treatment your shoes will be sterilised with a UV laser. It is highly recommended that you either wash all of your old socks with an antifungal wash or you get a new set to prevent reinfection.
Get treated for fungal nails in Brisbane or Mt Isa
The first step in getting rid of your fungal nails is to come in and see one of our friendly podiatrists for an initial consultation. We will thoroughly assess your nails to determine which type of treatment is best suited to you.


